May 27th 2020
Dear Councillors and Officers,
We address Coventry and Warwickshire Joint Health Overview and Scrutiny Committee members and officers in attendance at the most recent meeting (January 22nd 2020). We would be grateful if you could forward this to anybody who is a member of the Committee who has been omitted from this email.
We hope you and all your colleagues at Warwickshire County Council, Coventry City Council and Coventry and Warwickshire Joint Health Overview and Scrutiny Committee are well.
Members and supporters of the Coventry and Warwickshire Keep Our NHS Public Campaign Groups believe it is imperative that the Coventry and Warwickshire Joint Health Overview and Scrutiny Committee meet as soon as possible, virtually and in public, in order to scrutinise the government’s, the Coventry and Warwickshire Health and Care Partnership’s and the CCGs’ response to the Covid19 pandemic.
Although the government may claim that it has achieved its overriding goal, this has been at the expense of many people’s lives and wellbeing. On May 5th BBC News reported that the UK death toll was the highest in Europe (1)
As Dr Maria Van Kerkhove, Technical Lead, WHO, Infectious Disease Epidemiologist said:
“Asking the question “are we doing enough?” regularly and repeatedly is critical.”
We see the role of scrutiny as vital to transparency at this crucial time.
We need to ensure that the Nolan principles prevail under the wide-ranging and hastily legislated Coronavirus Act. We need the principles of objectivity, accountability, openness and leadership.
Below are issues we would like you to scrutinise, since they remain unresolved and problematic. Bringing accurate information about them into the public domain is vital for the formulation of a more effective response to Covid-19 than what we have at present.
We propose local primary care and public health systems must be central to the response to Covid-19
The first Independent SAGE online meeting of notable scientists from many relevant disciplines – including public health, computer modelling, behavioural science and intensive care medicine – revealed a strong consensus that local primary care and public health systems must be central to the response to Covid19.
Their report, COVID-19: What are the options for the UK? Recommendations for government based on an open and transparent examination of the scientific evidence (2) endorses the World Health Organisation guidance on transitioning from lockdowns.
The second of the six of the WHO requirements states that:
“Sufficient public health and health system capacities are in place to identify, isolate, test and treat all cases, and to trace and quarantine contacts.”(3)
What is happening?
We are aware that there are significant weaknesses in the government’s centralised and privatised test/trace/track scheme, which sidelines local NHS labs and public health professionals.
Testing
- a) Testing is too centralised. Many people who need tests cannot reach the testing centres. Can the Joint HOSC find out how many people cannot get tested because of transport/logistical problems.
- b) What is the justification for outsourcing testing from the NHS to private companies? Testing contracts have been given to private firms. In Coventry and Warwickshire, the Ricoh Arena testing centre has been contracted to Deloitte, which has subcontracted to Sodexo. Why?
- c) Test results analysis has by-passed NHS pathology labs, and been contracted to private-public partnership ‘Superlabs’. A statement by The Institute of Biomedical Science raises concerns about the quality of the service provided by these three new Lighthouse Labs:
“It is clear that two testing streams now exist: one delivered by highly qualified and experienced Health and Care Professions Council (HCPC) registered biomedical scientists working in heavily regulated United Kingdom Accreditation Services (UKAS) accredited laboratories, the other delivered mainly by volunteer unregistered staff in unaccredited laboratories that have been established within a few weeks.”(4).
- d) Where do the results go? After the tests are processed it is vital that the results are shared with local authorities’ public health departments and GPs. Without this information it is impossible for GPs and Councils’ Public Health Departments to put in place proper health care for Covid-19 sufferers, and effective virus suppression measures, including local contact tracing and isolation support. But, as the Health Service Journal reported on May 12th “Data on tens of thousands of tests not accessible to local NHS and councils; No data is being reported until further notice and Senior NHS source says national reporting has also stopped” (5)
Tracking and Isolating
The government is using private companies to start the tracking process. They are not delivering.
Serco. The government will use a centralised call centre system of around 21,000 tracers. It has outsourced this to SERCO, despite the Serious Fraud Office having conducted a criminal investigation into this company’s false accounting by fraudulent tagging in July 2019. Serco has already shown incompetence in ‘accidentally sharing contact tracers’ emails’.
Sitel: Training, run by contact centre company Sitel, is deficient. Trainees reported spending days just trying to log into the online system, virtual training sessions left participants unclear about their roles, new contact tracers were told to rely on a two-page script and a list of frequently asked questions, and were told to consult YouTube for advice on how to deal with a bereaved person (Guardian May 20th).
HR Go has been running recruitment. On May 18th it told applicants applying for contact tracing jobs that hiring ‘had been paused’, while the government denied this.(6)
The current centralised, private system is proving to be incompetent and failing. Meanwhile, the lockdown is being gradually lifted. Unless and until a proper system of local testing, tracking and isolating is in place, more people will die – unnecessarily.
Local, Community Based Testing, Contact Tracing and Isolating.
In some parts of the country, community run contact tracing has begun. Sheffield is one example (7).
Local KONP groups, including retired doctors, one of whom was Director of Public Health in South Warwickshire, are pressing the Coventry and Warwickshire Health and Care Partnership to support local Public Health directors to organise local, community led testing, tracing and isolation.
Tracing must be run by people in the community who know the community. It must be run by Public Health departments, GPs, retired health professionals, volunteers, environmental health experts and others.
We urge Coventry and Warwickshire Joint Health Overview and Scrutiny Committee to support us in making the Government accountable for its decisions in this pandemic, including the failures outlined above.
The Government press release https://www.gov.uk/government/news/300-million-additional-funding-for-local-authorities-to-support-new-test-and-trace-service on May 22nd that there is ‘£300 million additional funding for local authorities to support new test and trace service’ and that ‘Local authorities will be central to supporting the new test and trace service in England, with the government providing a new funding package of £300 million’ leaves local authorities still subordinated to the centralised testing and tracing policy.
Senior directors of public health have told the Local Government Chronicle that ‘they are still being kept in the dark on how government plans for track and tracing will be rolled out nationally, and have raised fears it will result in a “shambles” on the same scale as personal protective equipment (PPE) and Covid-19 testing’ (https://www.lgcplus.com/politics/coronavirus/directors-of-public-health-fear-shambles-over-contact-tracing-20-05-2020/). The LGC cites Coventry and Warwickshire Health and Care Partnership Chair, Sir Chris Ham, is highly critical of the government approach, stating in a Tweet, that ‘the government’s use of the private sector is “not working”, slamming the NHS tracing app “a sideshow” and calling on public health directors to take on a greater role’.
Coventry and Warwickshire Joint Health Overview and Scrutiny Committee can play a key role in backing the Coventry and Warwickshire Health and Care Partnership to fully support local Public Health departments, local public and environmental health services, councils, and GPs in establishing a local Coventry and Warwickshire COVID-19 Test, Track and Isolate system.
To start this, some immediate questions need asking and need answers.
Questions for the Joint HOSC to ask on Testing:
- Are the Directors of Public Health (DPH) at Warwickshire County Council and Coventry City Council receiving daily reports of numbers tested by testing site – (Ricoh Arena and any others)
- Are the DPHs informed of positive test results?
- Are GPs informed of positive results?
- How many results are going missing?
- Will DPH & Public & Environmental Health teams have any involvement in contact tracing or will it all be done by call centres?
Other key issues
In addition to local testing, contact tracing and support, we ask Coventry and Warwickshire Joint Health Overview and Scrutiny Committee to scrutinise the following key issues to suppress the spread of Covid-19 from now on:
- Covid-19’s disproportionate impact on poor and Black And Minority Ethnic communities and individuals and what measures must be taken to stop this.
- The effect of the mass hospital discharge of patients at the end of March of Covid-19 patients and deaths in care homes in Coventry and Warwickshire.
- Whether the understandable push for GPs to make sure that patients with a frailty score of 6+ have made Advanced Care Plans has been associated with any CCGs’ directives or encouragement to deny such patients access to hospital care in the event that they fall ill with Covid19.
- The lack of PPE which has risked and in too many cases taken the lives of NHS, social care workers and other key workers.
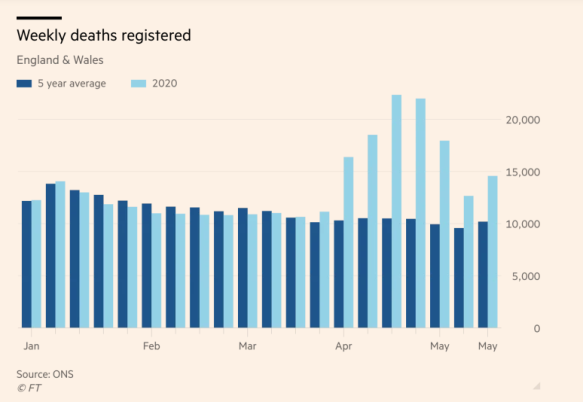
- The rise in ‘excess deaths’ that are not from Covid-19 but are probably the result of inadequate public information about “green” zones in GP surgeries and hospitals, so that people can safely attend for non-Covid-19 health problems.
- How “normal” NHS services are going to resume, including resumption of elective surgery.
- The cost and effect of the block contracts for NHS use of private hospitals in Coventry and Warwickshire.
- The funding needs of Councils for Covid-19 costs including loss of income through business closures etc.
The advice by the government’s Scientific Advisory Group for Emergencies (SAGE) has been challenged by many science experts, who have formed Independent Sage (9). We recommend the latter’s list of issues relating to the Covid-19 pandemic response:
- Transitioning from lockdown and closures
- Test, Trace, Isolate, Support, Integrate
- Minimise outbreak risks in high vulnerability settings
- Establish preventive measures in workplaces
- Ensure communities have a voice, are informed, engaged and participatory in the transition
- Effective clinical care for patients and staff
- Health, social and economic protections for women, marginalised and BAME groups
- What is needed for the future?
References.
Signed:
Dr. Gordon Avery formerly Director of Public Health, South Warwickshire
Martin Drew, Member, South Warwickshire Keep our NHS Public
Frances Hoch Retired SRN and Health Visitor, MA by Research Sociology of Health and Illness, University of Warwick, BScN (Hons) Specialist Community Public Health Nursing, University of Wolverhampton
Pat McGee Chair, Coventry Keep Our NHS Public
Dave Nellist, Secretary, Coventry Keep Our NHS Public
Professor Anna Pollert, Secretary, South Warwickshire Keep our NHS Public.
Professor Nick Spencer, Emeritus Professor of Child Health