Huffington Post August 20th 2020.
Firms with no history of supplying the products they were paid for, a business linked to Brexit lobbyists, and a dormant company were among the beneficiaries.
The coronavirus pandemic brought about an unprecedented peacetime public spending boom in the UK as the government pumped billions into trying to fight Covid-19.
But an investigation by HuffPost UK has led to renewed calls for an inquiry into government spending amid “scandalous and shocking” revelations about the way taxpayers’ money was handed out.
HuffPost UK has investigated which companies have profited from the pandemic that has killed 45,000 Brits and left millions at risk of redundancy.
We found deals involving “eye-wateringly large” sums of money that have proved highly controversial.
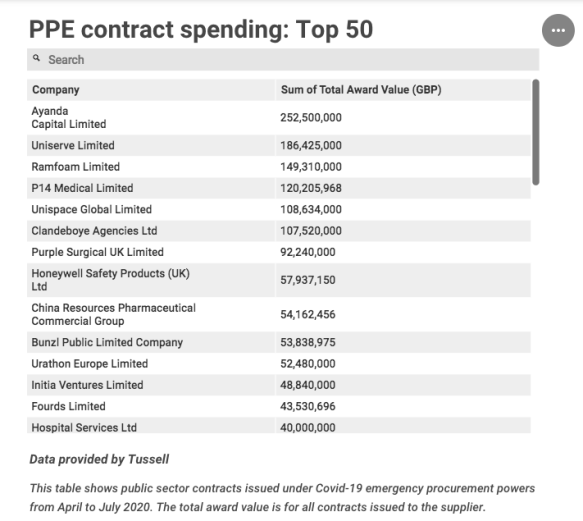
Revelations have already hit headlines about large PPE and testing contracts awarded to firms that ultimately supplied unsuitable products – such as Ayanda Capital Ltd and Randox – which has placed a spotlight on the government’s use of emergency procurement powers.
Now HuffPost UK can reveal other areas of government spending that raise further questions about how suppliers were selected and how these deals were arranged.
- We found that PPE contracts worth £186m, the second largest amount spent with any PPE supplier, went to UK logistics firm Uniserve Limited, whose multi-millionaire owner is listed as a speaker for the influential pro-Brexit lobby group Prosperity UK. Other speakers listed on the site include chancellor Rishi Sunak and cabinet minister Michael Gove.
- Another two large PPE contracts worth £49m in total went to a company, Initia Ventures Ltd, with assets of only £100. Companies House records list it as dormant.
- Of the 10 companies that were handed the highest value deals to supply the government with PPE, we found that five had no apparent record of procuring PPE previously.
- One firm told HuffPost UK its plan to manufacture face masks in the UK for as little as 10p a unit was turned down by government, despite its offer to make 75m masks a month at no profit at the point when the NHS need for PPE was at its most dire.
- Smaller UK testing companies also told HuffPost UK the process unfairly excluded them from winning orders and may have deprived the UK of vital tests at the peak of the pandemic.
- We found consultancy firm KPMG was paid almost £1m for three months’ work on one Nightingale hospital in Harrogate. This is the first time any information has come into the public domain about spending with top consultancy firms on the Nightingales. The government and NHS has faced criticism for its secrecy over the issue.
There is no suggestion of wrongdoing on the part of any of these companies.
In many cases, the thousands of firms that won Covid-19 contracts from government were at the forefront of the national effort to tackle the virus.
But these deals and others revealed in the data raise questions about how the government, moving at speed and during a period of incredibly intense global demand, decided which companies should be appointed as suppliers.
Under the guidelines that are in place under emergency Covid-19 procurement powers, known as Regulation 32 powers, government and other public authorities do not have to go out to competitive tender due to the need to appoint suppliers with “extreme urgency”.
However, it is unclear how the government sought to achieve best value for money without the usual checks and balances in place – for example, how the Department of Health and Social Care (DHSC) would have selected a dormant company such as Initia Ventures Ltd, which has no history manufacturing PPE, as a supplier when it was not carrying out tendering processes.
“There must be an inquiry into the way government has handled the crisis and into the way public money has been spent,” said MP Rosie Cooper, who sits on the health and social care committee.
“It is scandalous and shocking that eye-watering sums of money appear to have been spent with companies that don’t have a track record in this field, such as PPE and test and trace.
“Disgracefully, companies with experience were ignored, and government needs to explain how nearly £50m can be spent with a dormant company. Who authorised that and why?
“Why were smaller testing companies ignored while contracts were placed with large companies who failed to deliver? Who took each decision and why needs to be made public.”
She said taxpayers needed answers, adding: “It’s their money and they’re likely to be paying for these decisions for many years to come.”
A government spokesperson said proper due diligence was carried out for all contracts and collaborations with the commercial sector had strengthened the pandemic response.
“As a result of public and private sector organisations working together at pace, we were able to protect our NHS and strengthen our response to this unprecedented global pandemic,” he said.
But shadow health minister Justin Madders MP said significant questions remained about government accountability over this spending, with scrutiny vital because of the intense pressure coronavirus has placed on public sector finances.
“When we’ve got nurses, who have literally put their lives on the line for the last six months, protesting on the streets because they haven’t had a decent pay rise for a decade, you’ve got to ask whether all the money that’s been put into this has been spent wisely,” he said.
“And of course when a government is faced with decisions like that, it’s only right that every item of government expenditure is closely examined.”
Spending on personal protective equipment
HuffPost UK analysed data on all public sector spending under emergency Covid-19 procurement powers from March to July this year, to find out which firms won out in the government’s pandemic spending boom.
The data provided by Tussell, a company that publishes information on UK government contracts, shows industries supplying products and services vital to battling the pandemic – such as personal protective equipment (PPE) and testing – have seen the highest level of spending.
The contracts issued to buy PPE in particular have proved highly controversial, already causing a mounting political row. The data show 471 PPE contracts were published from April to July, totalling £2.6bn.
HuffPost UK found firms who, on paper, appeared to have no record in manufacturing or supplying PPE were among those awarded huge contracts worth in some cases hundreds of millions of pounds of taxpayers’ money.
Five of the 10 PPE suppliers with whom the government spent the most money – £709m in total – were companies that had no apparent background in supplying PPE.
One of those firms was Upminster based logistics and global trade management company Uniserve Limited, which won five contracts in April worth £186m – the second highest amount paid to any one company for PPE. The contracts were to supply gowns, gloves, aprons, face masks, face shields, and protective goggles.
Questions have been raised about Uniserve’s connections to central government.
In 2018, the firm was appointed as a UK government adviser on tech and customs, according to its website, and its owner and founder Iain Liddell is listed as a speaker for the influential pro-Brexit lobby group Prosperity UK, which is linked to a number of leading Brexiteer MPs.
Other Prosperity UK speakers listed on the site include chancellor Rishi Sunak, former business secretary Greg Clark, former Brexit secretary David Davis, and chancellor of the Duchy of Lancaster Michael Gove.
The government said ministers were not involved in the awarding of contracts, so any connection through Prosperity UK had no bearing on the Uniserve deal.
Uniserve did not comment.
Contracts worth £49m also went to a company called Initia Ventures Limited, which is listed as having assets of only £100 and in January 2020 was marked as dormant on Companies House.
HuffPost UK could find no website for the company, which is registered at the address of its accountant in Finchley, north London.
Despite the firm having no apparent trading history or background supplying PPE, DHSC awarded it one contract for isolation suits worth £32.6m on April 19 at the peak of the pandemic, and then another worth £16.3m just five days later on April 24.
The company’s director Amogh Kalyanpur said it had provided “various levels of security and de-risking to the DHSC along with a highly credible manufacturer”, which he believes allowed it to win the contracts.
“Yes, we did not have a history in the UK but the track record is in the businesses and manufacturers we are working with in China, Thailand, Hong Kong and India – which is where the goods are manufactured and which is also the bottleneck for logistics,” he said.
“None of our shipments have faced any of these issues or quality issues. And this is down to the team we have on the ground and the credibility of the manufacturer – with whom we have had an exclusivity for representation in the UK from the outset.”
He said the bid was made directly to the procurement team for the Covid-19 response and not through any contacts, political or governmental.
HuffPost UK asked DHSC how the Uniserve and Initia Ventures contracts were agreed.
The government said both companies had responded to a public call to action over PPE and went through the same due diligence as all suppliers who made bids.
My wife’s a GP and she managed to get Covid because their [health] trust were told to just go out and buy whatever they could. They shouldn’t be expected to be doing that
But other companies that missed out in this process have questioned the efficacy of the system.
One firm that offered the government the opportunity to manufacture Type IIR surgical face masks, which have the highest level of filtration, directly in the UK for only 10p a unit says its bid was rejected despite the NHS experiencing desperate shortages of PPE at the time.
Market prices for this type of mask were averaging 59p to 64p a unit in April, according to government.
Total Productivity Solutions Ltd bid in early May to set up a UK manufacturing plant to produce face masks, guaranteeing that it had the equipment and necessary raw materials to do this.
The company says its proposal would have allowed the government to produce 75m masks a month cheaply, quickly and without paying manufacturers’ profit, and the facility would have been up and running within six weeks if the bid had won approval, guaranteeing supply.
The pitch went in at a time when the government was agreeing riskier deals with companies such as the £253m contract with Ayanda Capital Ltd, an investment firm that had no PPE experience, which resulted in the purchase of 50m masks that were not unusable.
Nik de Villiers, senior partner at Total Productivity Solutions, said: “If you compare our solution, for the same money that was spent you could have actually manufactured a billion Type IIR masks. So on paper it’s really not comparable.
“Had we been given the go ahead back in May, we would have been up and running a serious production facility now that would be producing British-made masks of the highest quality that would be good enough for the NHS,” he continued.
“My wife’s a GP and she managed to get Covid because their [health] trust were told to just go out and buy whatever they could. They shouldn’t be expected to be doing that – they should be given the right tools to carry out their jobs.”
The company is now in talks with Amazon about taking the proposal forward, but says its preference would have been to supply the NHS.
“Amazon has indicated to us that our proposition will be by far the cheapest that they’ve seen that actually fits the standard of quality that they require,” said de Villiers. “But our preference has always been to do it for the government.”
DHSC did not comment on the bid but said its focus was on working with companies that could have the biggest immediate impact on protecting frontline workers.
The data also shows that DHSC awarded contracts worth a total of £755m to 41 companies with “caution” or “high risk” credit indicators.
These include three of the highest value contracts with Ayanda Capital; P14 Medical Limited, which is owned by a Conservative councillor; and confectioners Clandeboye Agencies Ltd. All three have credit indicators of “caution”.
The sheer volume and variety of companies providing PPE revealed in the data points to the intense pressure the government was under to secure supplies as it looked outside of established supply chains at the height of the pandemic.
It also raises questions about why more PPE had not been stockpiled earlier and crucially whether lives might have been saved had the proper equipment been available sooner.
The Labour Party has now formally requested a probe by the National Audit Office into contracts awarded under emergency Covid-19 powers that bypassed competition rules due to urgency.
Rachel Reeves MP, shadow minister for the Cabinet Office, said: “There is concern from the public but also from within the business community at some of the peculiar procurement decisions made by the Conservative government without goIng out to tender.
“Labour has called for the National Audit Office to investigate the government’s approach to procurement so that there can be transparency, public confidence and a more effective approach taken in the crucial months ahead.”
Spending on Covid-19 testing
The data on testing contracts handed out by Whitehall paints a similar picture about the government’s preparedness.
From March to July this year, 109 testing contracts worth £1.5bn have been published across the public sector.
In marked contrast to the PPE deals, the government has relied largely on established big pharma companies to provide testing, with three firms owned by US pharmaceutical giants featuring on the list of top suppliers.
HuffPost UK found some of the largest deals were awarded by DHSC, which has contracted out £646m in testing services since early March, and has relied heavily on multinationals.
 The highest value contract, worth £151m, went to Hologic Ltd for the supply of coronavirus tests to laboratories across the UK. The Manchester-based company is ultimately owned by US pharmaceutical giant Hologic Inc in the US, which is expected to see bolstered revenue growth from testing sales this year.
The highest value contract, worth £151m, went to Hologic Ltd for the supply of coronavirus tests to laboratories across the UK. The Manchester-based company is ultimately owned by US pharmaceutical giant Hologic Inc in the US, which is expected to see bolstered revenue growth from testing sales this year.
Contracts worth £68m were issued to Life Technologies Limited, which is ultimately owned by Thermo Fisher Scientific Inc – another pharma giant in the States. The US firm reported that its quarter two revenues for the year have soared by 10% driven by pandemic demand.
A £28m contract went to the UK firm Oxford Nanopore Technologies Ltd, which won a deal to supply test kits, training material and support.
The company was founded in 2005 as a spin-off from the University of Oxford. It is now one of a tiny group of what are called “unicorn” start-ups because they are rare in having grown to a value exceeding $1bn.
Swiss pharma giant Roche also won contracts worth £34m with Public Health England through its UK arm Roche Diagnostics Limited. Its machines and kits are used to process coronavirus tests in laboratories.
But smaller UK-based testing companies claim they were unfairly left out of the process, with the government being unduly reliant on large multinational companies to the detriment of supply.
Pro-Lab Diagnostics Ltd manufactures test kits and reagents. It won contracts worth £6.1m to supply kits to NHS labs – but its general manager Mark Reed said lots of other small and medium sized businesses felt locked out of the process.
Reed, who sits on the board of industry group the British In Vitro Diagnostic Association, told HuffPost UK: “I do know that some of my friends in the industry have been extremely vocal about how they felt it was unfair that competitive tenders weren’t issued and evaluations were done behind closed doors.
“Now, we were fortunate because we positioned ourselves very well and we did get awarded a contract. But as time has moved on, there does seem to be a bit of a lean towards: ‘Let’s talk to the big boys first, and then we’ll talk to the medium-sized companies.’
“You can’t deny that there does seem to be a bit of favouritism towards these huge multinational corporations.”
It has caused even greater anger within the industry as there have been issues with some of the bigger deals – such as a £133m contract with Randox Laboratories Ltd. Last month the government ordered a pause on the use of Randox test kits saying some may not meet required safety standards.
Pro-Lab said it hasn’t reached full capacity of manufacturing a million tests a week, never getting above 400,000, and that it is now in a position where NHS labs are wanting to place orders but a block is occurring because of the bureaucracy of the central system.
Charlotte Duncan, the firm’s technical director, said: “It is very frustrating and it does feel very much like you’re just permanently banging on doors. The drive is coming very much from our customers.”
HuffPost UK found the largest single testing contract issued was by the Treasury, which awarded £750m to the Office for National Statistics to set up a Covid-19 infection survey.
The survey is being carried out to try and understand how many people in the UK have Covid-19 and the ONS has alerted the market to the fact that it will award one or more commercial contracts to work on the survey.
No further information is yet available about which firm, or firms, have been or will be appointed, and the ONS did not comment when asked by HuffPost UK.
But this could potentially end up being one of the largest set of contracts with the private sector under the emergency Covid-19 spending powers.
Another of the largest deals was the huge £108m NHS Test and Trace contract handed to outsourcing giant Serco, which has announced its profits soared by 53% in the first six months of the year.
The data also reveal the well publicised contract awarded to Amazon to provide postal services to deliver coronavirus tests was worth £8m.
Spending on the Nightingale hospitals
Another area of significant public spending under emergency Covid-19 powers is on the NHS Nightingale hospitals.
The pop-up hospitals were constructed inside existing buildings in the first weeks of lockdown so the NHS would not be overwhelmed by the pandemic, and were the flagship policy in the government’s early response to Covid.
Contracts published to date show NHS England awarded £346m to hospital trusts to set up the Nightingales, but no information is yet available about the private firms that were paid in turn to actually build the hospitals.
Using hospital trust spending records, HuffPost UK has established that the consultancy firm KPMG was paid £923,000 over three months for what are described as “audit fees” related to the construction of just one of the Nightingale hospitals in Harrogate.
KPMG says it did all Covid-19 contract work at cost price. NHS England did not comment on the deal.
But questions have gone unanswered about the role that consultancy firms played in the building of the Nightingales and in July the powerful Public Accounts Committee (PAC), which holds the government to account over spending, slammed the lack of transparency.
The PAC said: “We are concerned by the scarcity of information on contracts and costs. When asked, NHS England and NHS Improvement was unable, or unwilling, to provide any estimate of the cost of private sector capacity or the Nightingale hospitals.”
The PAC said it was “imperative” the DHSC and NHS provide information about costs and “how the Nightingales have been used and will be used in coming months”.
HuffPost UK reported onsecrecy surrounding these contracts, and calls for the government and NHS England to be more transparent, in June.
The figures that are available show the Nightingale West Midlands hospital in Birmingham cost almost twice as much as any of the other hospitals to build, at £109m.
The contracted costs for the other Nightingale hospitals varied from £20.3m for the Devon and Cornwall hospital to £55.8m for the Nightingale Excel in London.
NHS England has not commented on how much it will cost to keep the facilities – which are based in privately owned buildings such as the Excel conference centre in the capital’s Docklands area, and the NEC in Birmingham – open and operating.
The government says the Nightingale hospitals will be repurposed as cancer testing centres, with most only ever having admitted a handful of coronavirus patients.
Why is this important?
Procurement experts acknowledge there was a need for the emergency Covid-19 spending powers, which relaxed competition rules due to the urgency of responding to the pandemic.
But this does not reduce the need for the government to be accountable for its decisions, which is why there have been mounting demands for an inquiry.
Experts say the perception of fairness and transparency in how large public contracts are awarded is vital in maintaining public confidence in government.
Duncan Hames, director of policy at Transparency International UK, said: “It is incumbent on the government to prove it is delivering value for money, not just giving money to those it values. Allegations of cronyism can do untold damage to public confidence in its response to the pandemic.”
The amount spent by the public sector through emergency Covid-19 procurement has been colossal – with 1,188 contracts published from March to July totalling £5.8bn of taxpayers’ money.
Critically, every extra pound spent on PPE or testing contracts that could have been won at cheaper or more competitive prices also leaves less in the public purse at a time of significant spending pressure on the NHS, schools, and the welfare state.
To put some of the huge figures in context, chancellor Rishi Sunak allocated £25bn just for PPE and the government’s Test and Trace scheme in his coronavirus budget in July. This sum almost equalled the £30bn allocated to kickstart the UK’s economic recovery from the Covid-19 crisis.
The £755m the DHSC spent buying PPE from companies with caution or high-risk credit indicators was more than the £750m committed by the chancellor to support all frontline charities in the UK to keep delivering services during the coronavirus outbreak.
Dr Wanda Wyporska, executive director of The Equality Trust, said the revelations over some of the Covid-19 emergency spending would exacerbate the perception of one set of rules for government and another for everyone else.
“Many people face huge levels of conditionality for the money they receive as welfare payments. If they were late for appointments or failed to turn up at the job centre then they would quickly see payments docked,” she said.
“This has tipped many into poverty, homelessness and debt. However, it’s a different story when vast amounts of taxpayers’ money is being handed out to big companies without much conditionality or even checking.
“As Covid-19 exacerbates the already damagingly high levels of inequality in the UK, we must really ask what plans the government has for fulfilling its commitment to the United Nations Sustainable Development Goal 10 – reducing inequality.”

